Essential Components of Medication Therapy Management (MTM)
A. Patient and pharmacist relationship
1. Pharmacists have historically been viewed as one of the most trusted professionals based on Gallup’s annual Honesty and Ethics Survey. Pharmacists are also one of the most accessible health care professionals. Patients express greater satisfaction with care when they perceive quality interactions with a health care provider.
2. The provision of face-to-face MTMS strengthens the patient–pharmacist relationship. Although some MTMS can be provided via a phone interaction, face-to-face interaction with the pharmacist affords the ability for the pharmacist to observe visual signs and symptoms as well as changes in the patient’s status and well-being.
3. For optimum patient care to occur, pharmacists need to be culturally competent and aware of the patient’s level of health literacy.
- Cultural competency means the pharmacists are cognizant of their patients’ diversity regarding beliefs, values, behaviors, and language. Barriers in these areas can lead to miscommunication and poor health outcomes.
- Health literacy is an individual’s ability to obtain, understand, and follow directions related to his or her health care. According to the U.S. Department of Education, 9 out of 10 Americans have limitations regarding health literacy. Patients with poor health literacy generally have poor health status and are more likely to have medication-related problems. The Rapid Estimate of Adult Literacy in Medicine–Revised (REALM-R) is a simple and quick tool that pharmacists can use to assess patient’s health literacy. Pharmacists need to adapt their counseling and MTMS based on the patient’s health literacy level.
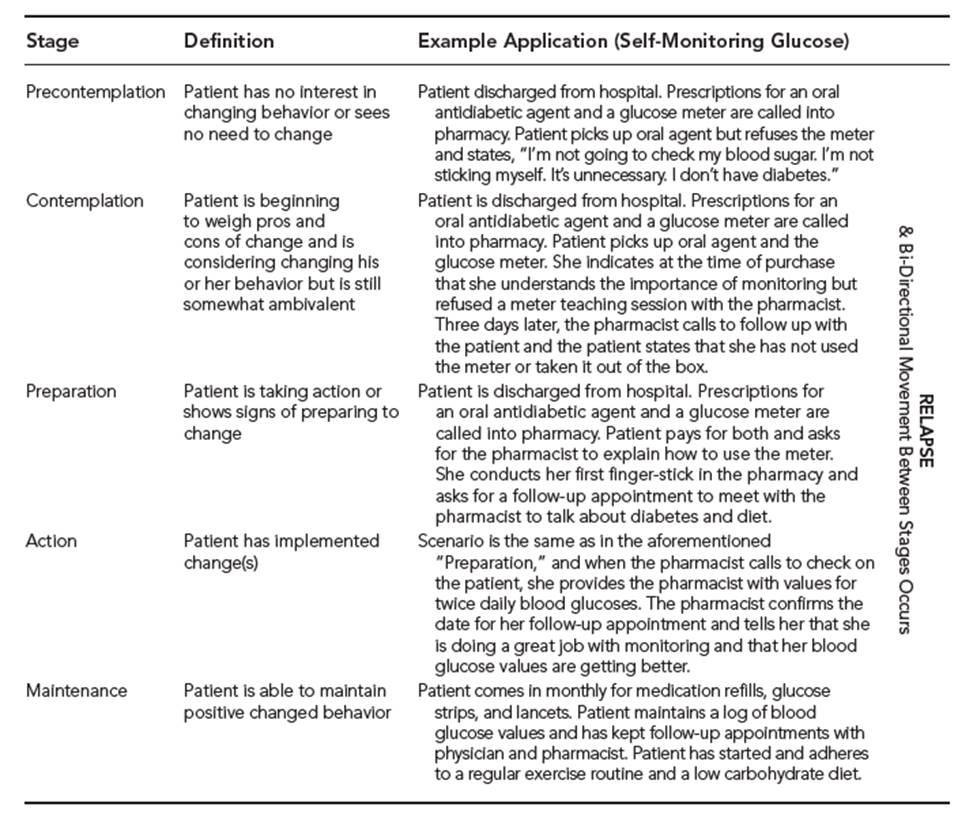
4. Successful MTM requires patient participation. Many MTM-related interventions require lifestyle or behavioral changes. Pharmacists need to assess their patients’ willingness to participate and change. Pharmacists should know the stages of change delineated within the Transtheoretical Model of Behavior Change (see below table). Pharmacists can also use a 0-to-10 visual analog scale for assessing a patient’s willingness to change. Scores $ 5 suggest the patient is willing to change and should be supported and encouraged.
B. Patient/caregiver interview
Depending on the patient, it may be appropriate for the pharmacist to include a caregiver in the patient interview.
- Interview setting
- A semiprivate or private area is required for the provision of MTMS. For interviewing purposes, the more private the area, the fewer interruptions and the more likely the patient will share and retain pertinent information.
- The interview area should have adequate lighting and a comfortable temperature. The space should be equipped with a table and chairs. The chair for patients should have arms to assist the patient in lowering to and rising from a seated position. The space should be large enough to accommodate the pharmacist, patient, and possible caregiver. In addition, the space should be readily accessible to patients with mobility problems (e.g., wheelchair, walker).
- The space should be relatively quiet to facilitate conversation (e.g., ability to close a door to the space, no ringing phone). Many MTM patients are elderly and have hearing deficits. Failure to create an environment where background noise is minimized may escalate patient’s frustration in communicating and adversely affect the desired outcomes.
- Essential technique
- Use open and honest communication: Introduce yourself; Explain the purpose and process of the MTM session; Ask for the patient’s expectations, concerns, and/or issues to be addressed.
- Avoid using and be aware of patients’ incongruent body language (i.e., mismatch in verbal and nonverbal language).
- Maintain good eye contact throughout the interview.
- Conduct the patient interview at the patient level. Avoid medical jargon.
- Ask purposeful questions.
- Use a combination of open- and closed-ended questions. Open-ended questions cannot be answered with a simple yes or no and generally begin with who, what, when, or how.
- Avoid rapid-fire questioning. Allow the patient time to answer a question before posing a second question.
- Avoid leading questions, for example, “You take your cholesterol medicine at night, right?”
- Use probing questions. Example: Questions asked to help elicit specific information from the patients regarding their medication therapy needs and problems.
- Use non defensive phrasing. For example, patients may become defensive with “why questions.” Instead of asking “Why did you not take your blood sugar medicine?” ask “What caused you to not take your blood sugar medicine?”
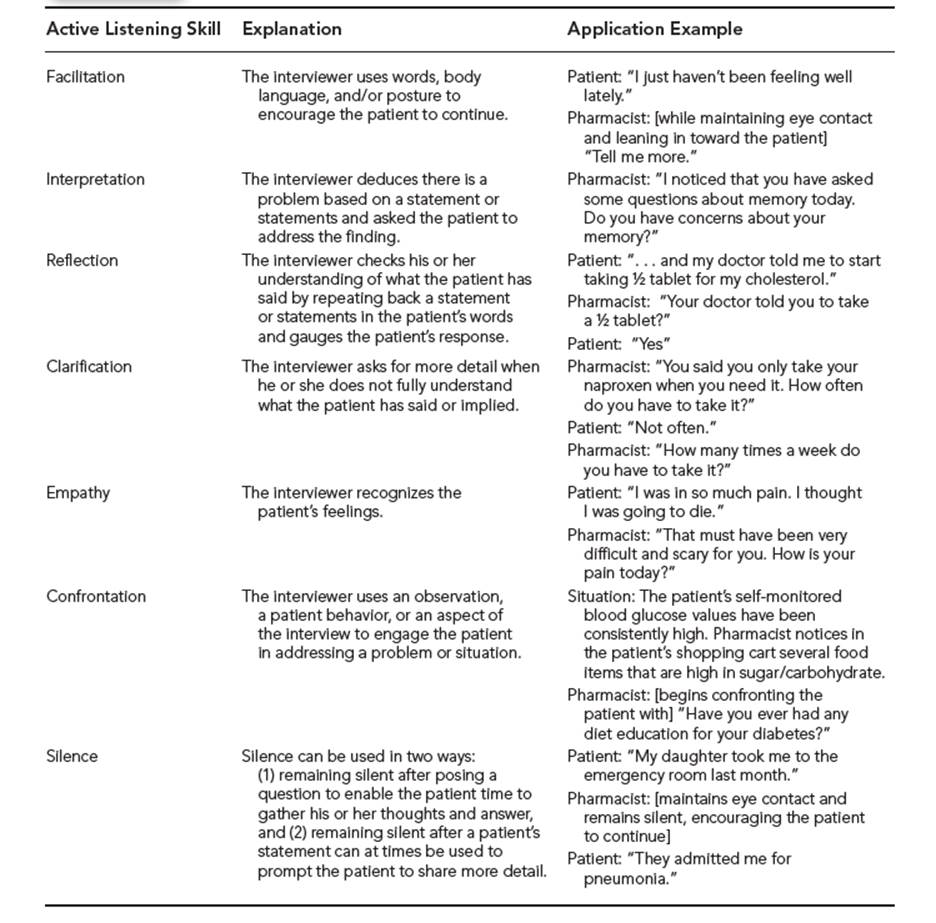
- Use active listening skills (see below table).
- Communication strategies for patients with disabilities. Patients with disabilities are capable of patient-centric care and should be empowered to be active participants.
- For patients with hearing deficits, remember to use a lower tone of voice and slower rate of speech. Use simpler sentences and sit directly across from the patient to facilitate lip-reading. Verbal education should be augmented with written materials. Consider providing and making available to your patient a sound amplifier.
- For patients with visual deficits (e.g., presbyopia, cataracts, glaucoma, macular degeneration, color blindness), clear and concise verbal communication becomes critical. When written communication or materials are necessary, these should be printed on nonglare, off-white, or pastel-colored paper. The font should be 14 points or greater in size; and avoid the use of yellow, green, and red.
- For patients with mental or cognitive deficits, the interview and education sessions may likely require the presence of a caregiver. Remember to always address the patient. Provide simple communication. Augment with simple written material.
- Essential components
- The content gathered during a patient interview is essential to enable a comprehensive assessment. The outcome of MTMS depends on the quality of information and data that pharmacist has available. It takes a considerable amount of time to do a thorough patient interview as indicated by the following components. To improve efficiency, the pharmacist may have the patient complete or provide information in advance or train a technician to assist with data collection.
- Basic patient demographics (e.g., name, date of birth, address)
- Chief complaint or reason for evaluation. In addition, it is helpful to ascertain what the patient/ caregiver wishes to accomplish by the MTMS. In other words, what are the patient/caregiver’s expectations?
- Health care priority. Comfort, cost, or convenience
- Past medical history, including surgeries and procedures, as well as any recent hospitalizations or emergency department visits
- Preventative health information such as immunizations and health screenings (e.g., colonoscopy, Pap smear, mammogram, prostate examination)
- Family history
- Social history that includes caffeine, nicotine, alcohol, prescription or illicit drug abuse, exercise, diet, occupation, and support network
- Allergies
- Medication history
- Vitals and lab values
- Review of systems
- Contact information for all prescribers and insurance information
- The content gathered during a patient interview is essential to enable a comprehensive assessment. The outcome of MTMS depends on the quality of information and data that pharmacist has available. It takes a considerable amount of time to do a thorough patient interview as indicated by the following components. To improve efficiency, the pharmacist may have the patient complete or provide information in advance or train a technician to assist with data collection.
C. Medication therapy review (MTR)
The MTR is conducted to determine appropriateness of therapy. The pharmacist should concentrate on necessity, safety, and efficacy of therapy. A useful outcome of the MTR is the detection/creation of a problem list (i.e., medication-related problems).
- Basic components of an MTR can be found within the medication appropriateness index, which helps to provide a systematic approach to the MTR.
- Is there a justification/indication for the medication?
- Is there any allergy or contraindication for the medication?
- Is the medication or regimen being used the most efficacious?
- Is the dose (age/condition) appropriate?
- Are the directions optimized?
- Are necessary monitoring parameters/practices in place?
- Is the duration of use appropriate?
- Are there any therapeutic duplications?
- Are there any drug–drug interactions? Drug–food? Drug–disease?
- Are there more cost-effective therapies available?
- Is the patient adherent with therapy?
- Are there any untreated conditions?
D. Therapeutic planning
The problem list created from your systematic MTR is used to create a therapeutic plan.
- The plan should be patient-centric, and with MTM for Medicare Part D, the plan is referred to as the Medication Action Plan.
- The therapeutic plan is designed to prevent, alleviate, and eliminate medication-related problems.
- The plan should be written to serve as documentation for services provided.
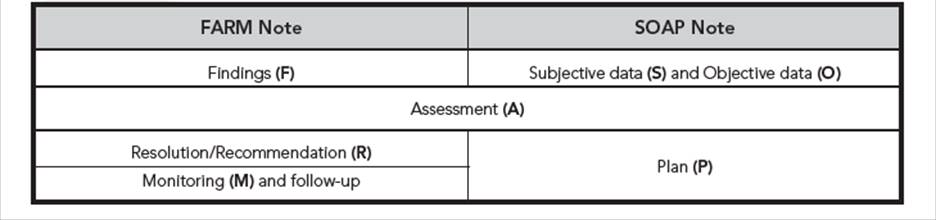
- Pharmacists may choose to use a traditional SOAP or FARM format for their documentation (see below table).
- Ideally, therapeutic plans should include the following:
- Goals for therapy
- The patient’s status on desired outcomes
- Recommendations for intervention
- Recommended monitoring parameters
- Desired time frame for follow-up
- Contingency plans for treatment may also be included in the event that treatment goals are
- not reached.
- Without appropriate follow-up, even the best of therapeutic plans are likely to fail. The success of therapeutic plans also depends on patient adherence, which is why this process should be patient-centric.
- The therapeutic plan required for Medicare Part D beneficiaries (i.e., MAP) should be developed in collaboration with the patient and should contain action items for which the patient is responsible.
E. Patient Medication Record (PMR)
After a comprehensive MTM, patients should be provided with PMR containing list of all of their medications, doses, directions, indications, any precautions, and start/stop dates. The patients should be instructed to present their PMR to all health care providers. The pharmacist should assist the patients in updating their PMR regularly and upon changes to the patient’s regimen.
Read also:




